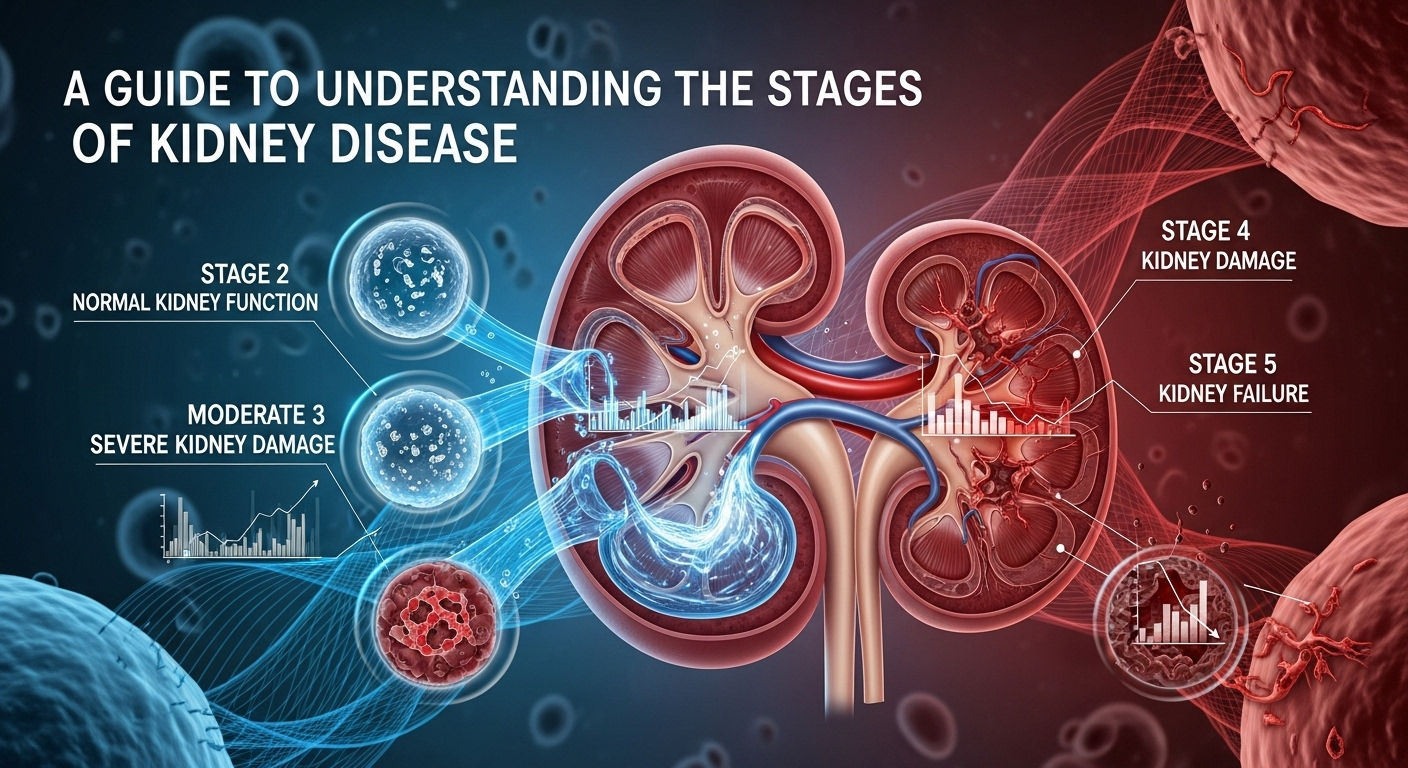
Your kidneys are among the body's most vital and hardworking organs. Functioning as sophisticated filtration systems, they tirelessly cleanse your blood, manage fluid balance, regulate blood pressure, and support bone health, all while operating silently in the background. However, when their function begins to decline gradually over time, a condition known as Chronic Kidney Disease (CKD) can develop. This condition is often progressive, moving through distinct phases that can be confusing and alarming. Gaining a clear and comprehensive perspective is the first and most crucial step toward managing the condition effectively. This comprehensive guide is designed to demystify the process, providing a clear path to understanding the stages of kidney disease and empowering you with the knowledge to navigate your health journey. What is Chronic Kidney Disease (CKD)? Chronic Kidney Disease, often abbreviated as CKD, is a long-term condition characterized by the gradual loss of kidney function over months or years. Unlike Acute Kidney Injury (AKI), which involves a sudden loss of kidney function, CKD is a slow and often silent decline. The primary role of the kidneys is to filter waste products and excess fluid from the blood, which are then excreted in the urine. When the kidneys are damaged, they become less efficient at this filtration process, leading to a build-up of waste and fluid in the body that can cause a cascade of health problems. The importance of the kidneys cannot be overstated. Beyond filtration, they perform several critical functions: Regulating blood pressure by managing fluid levels and releasing hormones. Producing an active form of Vitamin D, which is essential for bone health and calcium absorption. <strong>Controlling the production of red blood cells</strong> through the hormoneerythropoietin*. Balancing the body&#x27;s electrolytes, such as sodium, potassium, and phosphate. When CKD develops, all of these functions can become impaired. The disease is "staged" based on the level of kidney function remaining. This staging system helps doctors determine the severity of the disease, predict its rate of progression, and develop an appropriate management plan. By understanding which stage you or a loved one is in, you can better grasp the immediate health priorities and the long-term outlook, making you an active participant in your own care. The Key Metric: Understanding Glomerular Filtration Rate (eGFR) The cornerstone for staging kidney disease is a measurement called the Glomerular Filtration Rate, or GFR. The glomeruli are tiny filters within your kidneys—millions of them—that perform the initial step of cleaning your blood. The GFR is a measure of how much blood these filters clean each minute. A healthy pair of kidneys can filter approximately 120 milliliters (mL) of blood per minute. A direct GFR measurement is complex, so doctors typically use a formula to calculate an estimated Glomerular Filtration Rate (eGFR). To calculate your eGFR, your doctor will order a simple blood test that measures the level of creatinine, a waste product generated from muscle metabolism. This creatinine level is then plugged into a mathematical formula along with other variables like your age, sex, and body size. Historically, race was also a factor in the calculation, but modern guidelines are moving away from this practice to promote health equity and improve accuracy. The resulting eGFR number gives your healthcare provider a clear and reliable estimate of your kidney function percentage. The eGFR is the single most important number for staging CKD. Think of it as a percentage score for your kidneys. An eGFR of 75 means you have approximately 75% of your kidney function. As the eGFR number decreases, it signifies that the kidneys are becoming less effective at their job. This number allows doctors to classify the disease into one of five stages, track its progression over time, and make critical decisions about treatment, diet, and when to prepare for advanced therapies like dialysis or transplantation. A Detailed Breakdown of the 5 Stages of Kidney Disease Understanding what each stage means is vital for managing expectations and taking the right actions at the right time. The stages are primarily defined by the eGFR level, but the presence of kidney damage (such as protein in the urine, known as albuminuria) is also a critical factor, especially in the early stages. Stage 1: Kidney Damage with Normal or High GFR In Stage 1 CKD, the eGFR is 90 mL/min or higher, which is considered normal or even high kidney function. A person is only diagnosed with Stage 1 if they have other markers of kidney damage. This evidence could be the persistent presence of protein or blood in the urine, abnormalities detected on an ultrasound or CT scan (like polycystic kidney disease), or a family history of genetic kidney disease. Essentially, the kidneys are still working at or near full capacity, but there is underlying damage that signals a problem. Because kidney function is still good, symptoms are almost always absent in Stage 1. Most people are completely unaware they have a problem unless it is discovered incidentally during routine urine or blood tests for another condition. The primary goal of management at this stage is not to treat kidney failure but to aggressively manage the underlying cause of the damage to slow or halt its progression. This often involves strict control of blood pressure, managing blood sugar levels in people with diabetes, adopting a healthy lifestyle, and avoiding medications that can harm the kidneys (nephrotoxic drugs). Stage 2: Kidney Damage with Mildly Decreased GFR Stage 2 CKD is defined by an eGFR between 60 and 89 mL/min, coupled with evidence of kidney damage. This represents a mild decline in kidney function. Just like in Stage 1, the kidneys are still performing their essential tasks relatively well, and the body can effectively compensate for the slight loss in filtration capacity. It is a critical juncture where proactive management can have a significant long-term impact on the health of your kidneys. Symptoms remain rare in Stage 2, although some individuals might experience high blood pressure as one of the first signs of trouble. The focus of