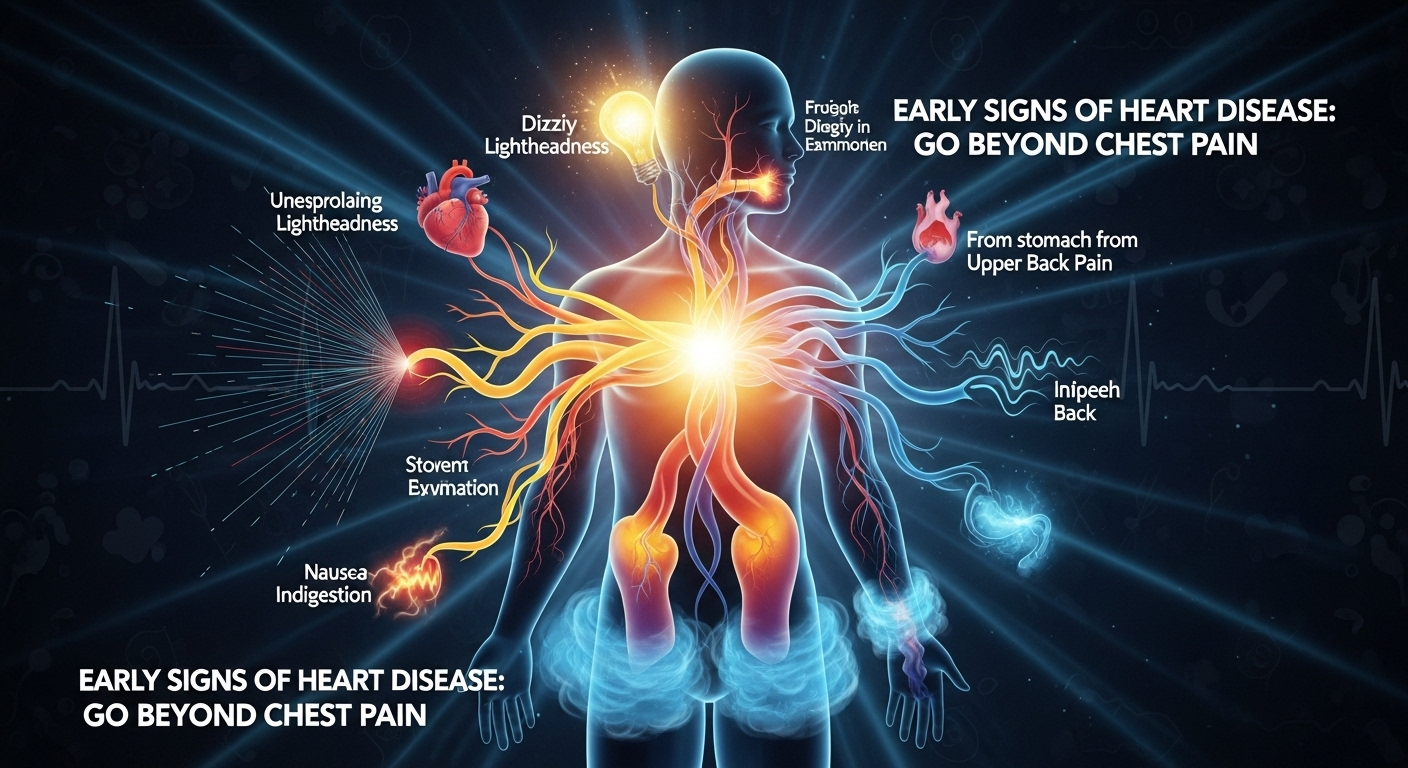
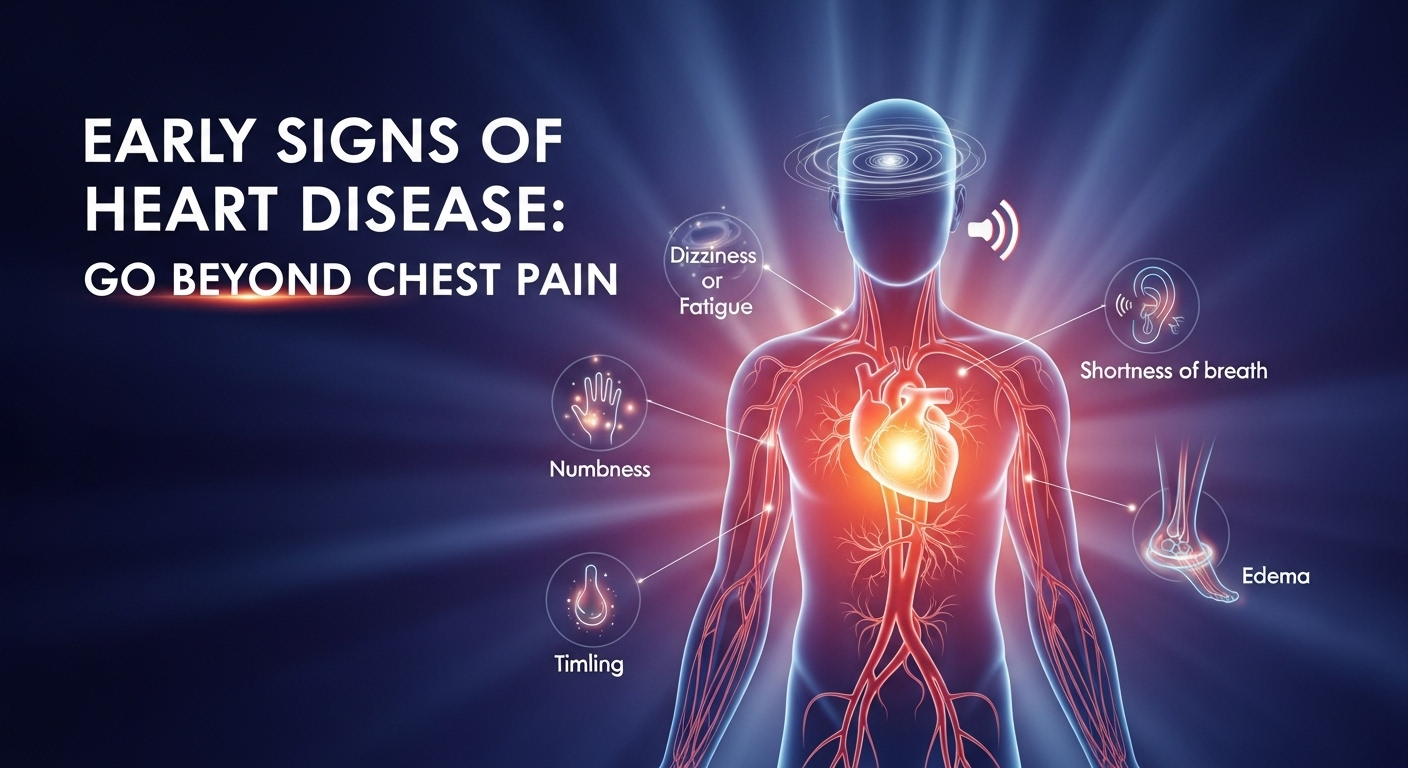
When you think of a heart attack, the image that often comes to mind is a dramatic scene from a movie: someone suddenly clutching their chest in excruciating pain. While severe chest pain is a critical sign, relying on it as the only indicator of heart trouble is a dangerous misconception. Many cardiovascular issues build up slowly over time, sending subtle, often confusing signals long before a major event occurs. Understanding what are the early signs of heart disease is crucial for early intervention and prevention. These whispers from your body can be easy to dismiss as signs of aging, stress, or a bad night’s sleep, but they are your heart’s way of asking for help. This article will guide you beyond the classic symptom of chest pain to uncover the less obvious, yet equally important, early warnings of heart disease.
Table of Contents
ToggleThe Classic Sign We Can’t Ignore: Understanding Chest Discomfort
While this article focuses on the less-obvious signs, it’s impossible to discuss heart disease without first addressing its most famous symptom: chest pain, medically known as angina. It’s important to understand that angina doesn’t always present as a sharp, stabbing pain. For many, it feels more like pressure, squeezing, fullness, or a heavy weight on the chest. This discomfort occurs when the heart muscle isn’t getting enough oxygen-rich blood, often due to narrowed or blocked arteries (coronary artery disease).
This sensation can be triggered by physical exertion or emotional stress and typically subsides with rest. However, there’s a more dangerous form called unstable angina, which can occur even at rest and is a sign of an impending heart attack. The pain might not be localized just to the center of the chest; it can radiate. Ignoring any form of chest discomfort is a significant risk, as it’s one of the most direct communications from your heart that something is wrong.
Differentiating heart-related chest pain from other causes like heartburn, muscle strain, or anxiety can be challenging. A key difference is that angina is often related to activity. If your chest feels tight every time you walk up a flight of stairs but feels better when you sit down, that is a major red flag. In contrast, pain that worsens when you press on your chest or take a deep breath is less likely to be heart-related. Regardless, self-diagnosis is never safe. Any new, unexplained, or worsening chest pain warrants an immediate conversation with a medical professional.
Subtle Signals: The Unexpected Early Warnings
Your heart is the engine of your body, and when it starts to struggle, the effects can be felt in surprisingly distant and diverse ways. These symptoms are often the true “early” signs because they can appear months or even years before a cardiac event. Learning to recognize these subtle signals is like learning a new language—your body’s language of distress. Paying attention can give you the crucial head start you need to seek treatment and make lifestyle changes.
Many people, particularly those who are otherwise active, might dismiss these signs as simply being “out of shape” or “getting older.” However, a sudden or unusual change in your body’s ability to perform daily tasks should never be taken lightly. Your baseline for what feels “normal” is your best guide. If activities that were once easy now leave you breathless or exhausted, your body is sending a powerful message that needs to be investigated.
These early warnings are your cardiovascular system’s check-engine light. They indicate that the system is under strain and not operating at peak efficiency. The sections below will break down these specific signs, explaining why they happen and what they feel like, so you can be better equipped to listen to what your body is telling you.
1. Unexplained Fatigue and Shortness of Breath (Dyspnea)
Feeling tired after a long day or a strenuous workout is normal. But the fatigue associated with early heart disease is different. It’s a profound, persistent exhaustion that isn’t relieved by rest. You might feel tired upon waking up or find yourself completely drained after simple activities like grocery shopping or making the bed. This happens because a weakening heart can’t pump blood as efficiently. To compensate, the body diverts blood away from less vital areas like your limbs and muscles to support critical organs, leaving you feeling chronically weak and tired.
Similarly, shortness of breath, or dyspnea, is a classic early sign. You might find yourself gasping for air after climbing a single flight of stairs or walking a short distance. This occurs for two main reasons. First, if your heart can’t pump blood effectively to the lungs, it can lead to fluid buildup, making it harder to breathe. Second, your body isn’t getting the oxygen it needs, so your lungs work overtime to compensate. If you experience shortness of breath while lying down that improves when you sit up, this is a particularly concerning sign of fluid in the lungs (pulmonary edema) and requires urgent medical attention.
2. Pain and Discomfort in Other Areas
The nerves from your heart share pathways with nerves from other parts of your body. When the heart is in distress, the brain can misinterpret the pain signals, causing you to feel discomfort in other locations—a phenomenon known as referred pain. This is why a heart attack doesn’t always manifest as central chest pain. Many people, especially women, experience pain in other areas instead of, or in addition to, chest discomfort.
Common areas for this referred pain include:
- The jaw, neck, or throat: Aching or tightness in the jaw is a surprisingly common symptom.
- The left arm or shoulder: This is the most well-known type of referred pain, but it can also occur in the right arm.
- The back: Pain or pressure between the shoulder blades is another frequent sign.
- The upper abdomen: Discomfort can mimic indigestion or heartburn.
The key is that this pain, much like angina, is often triggered by exertion and relieved by rest. If your jaw starts aching every time you go for a brisk walk, it’s far more likely to be related to your heart than a dental issue. Never dismiss persistent, unexplained aches in these areas, especially if they are linked to physical activity.
3. Dizziness, Lightheadedness, and Fainting (Syncope)
Feeling dizzy or lightheaded can have many causes, from dehydration to standing up too quickly. However, when it’s related to heart disease, it’s often due to a drop in blood pressure or an irregular heartbeat (arrhythmia). If the heart isn’t pumping strongly enough or its rhythm is off, it can’t circulate enough blood to the brain, leading to these sensations. In more severe cases, this can lead to fainting, known as syncope.
While a single, fleeting moment of dizziness might not be a cause for alarm, recurring episodes are a red flag. Pay attention to the context. Does it happen when you exert yourself? Does it come on suddenly without warning? Is it accompanied by other symptoms like heart palpitations (a feeling of a racing, fluttering, or pounding heart)? Dizziness combined with chest pain or shortness of breath is a medical emergency and requires immediate help. These symptoms could indicate a serious arrhythmia or a blockage that is severely compromising blood flow.
4. Swelling in the Legs, Ankles, and Feet (Edema)
When your heart’s pumping power declines, it can struggle to move blood effectively through your body. This causes blood to back up in the veins, leading to fluid retention. Gravity pulls this excess fluid down to the lowest parts of your body, causing swelling in your legs, ankles, and feet. This condition is known as peripheral edema. You might notice that your shoes feel tighter, or you can see indentations left on your skin after you take your socks off.
A simple way to check for this is the “pitting test.” Gently press your thumb into the swollen area for a few seconds. If an indentation, or “pit,” remains after you remove your thumb, it’s a sign of pitting edema, which is strongly associated with heart failure. Swelling can also be accompanied by sudden weight gain (a few pounds in a day or two) due to the excess fluid. While swollen feet can have other causes, new or worsening edema should always be evaluated by a doctor, as it’s a very common sign of a struggling heart.
Signs Often Overlooked, Especially in Women
It is a critical and life-saving fact that heart disease symptoms can present very differently in women compared to men. For decades, the “classic” heart attack victim was portrayed as a middle-aged man, and medical research often focused on this demographic. As a result, women’s symptoms were often misdiagnosed as anxiety, indigestion, or stress. Today, we know that women are just as likely to have heart disease, but their early warning signs may be far more subtle and confusing.
Women are more likely than men to experience the “atypical” symptoms discussed earlier, such as shortness of breath, back or jaw pain, and profound fatigue. In fact, for many women, crushing fatigue is the most prominent and debilitating symptom leading up to a heart attack. They may also experience symptoms that can be easily mistaken for a stomach bug or acid reflux.
These can include nausea, vomiting, and indigestion. A feeling of pressure in the upper abdomen, often dismissed as heartburn, can be a sign of a heart attack in women. Furthermore, women often report a profound sense of anxiety or impending doom—an overwhelming feeling that something is terribly wrong, even without clear physical symptoms. Recognizing this gender-specific presentation is vital for both patients and medical professionals to ensure timely diagnosis and treatment.
Understanding Your Risk and When to Take Action
Recognizing the early signs is the first step, but understanding your personal risk profile is just as important. Some risk factors are beyond your control, but many are directly influenced by your lifestyle choices. Knowing where you stand can empower you to take proactive steps to protect your heart health. A doctor can help you assess your risk and create a plan to manage it.
Don’t wait for a dramatic event to happen. If you are experiencing any of the signs discussed in this article, especially if they are new, persistent, or occur with exertion, it is time to see a doctor. It is far better to be evaluated and find out it’s a benign issue than to ignore a potentially life-threatening warning. Early detection and management are the most powerful tools you have against heart disease.
The table below outlines common risk factors for heart disease, separating them into those you can control and those you cannot. Focusing on managing the controllable factors can significantly lower your overall risk, even if you have uncontrollable ones.
| Controllable Risk Factors | Uncontrollable Risk Factors |
|---|---|
| High Blood Pressure (Hypertension) | Age (Risk increases with age) |
| High LDL (Bad) Cholesterol | Sex (Men are at higher risk earlier) |
| Smoking and Tobacco Use | Family History of Heart Disease |
| Diabetes (Type 2) | Post-Menopausal Status |
| Obesity and Excess Weight | Race/Ethnicity (Certain groups are at higher risk) |
| Sedentary Lifestyle (Lack of Physical Activity) | |
| Unhealthy Diet (High in processed foods, sodium, and saturated fats) | |
| Excessive Alcohol Consumption |
Diagnostic Tools: How Doctors Investigate Early Signs
If you present to your doctor with potential heart-related symptoms, they won’t just be guessing. They have a range of effective diagnostic tools to investigate the structure and function of your heart. Being aware of these tests can help demystify the process and reduce anxiety about your appointment.
A doctor will start with a physical exam and a thorough discussion of your symptoms and medical history. Based on that initial assessment, they may recommend one or more of the following tests:
- Electrocardiogram (ECG or EKG): This is a quick, painless test that records the electrical activity of your heart. It can detect abnormal rhythms, signs of a previous heart attack, or strain on the heart muscle.
- Echocardiogram: This is an ultrasound of the heart. It uses sound waves to create moving pictures of your heart, allowing doctors to assess the size of its chambers, the strength of its pumping action (ejection fraction), and the function of its valves.
- Stress Test: This involves monitoring your heart with an EKG while you walk on a treadmill or ride a stationary bike. It shows how your heart responds to physical exertion and can reveal blockages in the arteries that might not be apparent at rest.
- Blood Tests: A simple blood draw can reveal important information. Doctors will check your cholesterol levels (LDL, HDL), triglycerides, and look for specific proteins like troponin, which is released into the blood when the heart muscle is damaged.
- Coronary Angiography: This is a more invasive procedure where a special dye is injected into your coronary arteries. X-rays are then taken to reveal the exact location and severity of any blockages.
Frequently Asked Questions (FAQ)
Q: Can anxiety or a panic attack mimic the symptoms of heart disease?
A: Yes, absolutely. This is a very common point of confusion. A panic attack can cause symptoms like a racing heart, shortness of breath, chest tightness, and dizziness, which overlap significantly with heart attack symptoms. However, the pain from a panic attack is often described as sharp and stabbing, whereas heart pain is more often a pressure or squeezing. Also, panic attack symptoms tend to peak within 10 minutes and then subside, whereas heart attack symptoms are often more persistent. Despite the similarities, you should never assume its ust anxiety. Always seek medical evaluation for new or severe chest-related symptoms.
Q: At what age should I start worrying about my heart health?
A: Heart disease is not just a disease of the elderly. The processes that lead to it, like the buildup of plaque in the arteries (atherosclerosis), can begin in childhood. While the risk increases significantly after age 45 for men and 55 for women, it’s crucial to adopt a heart-healthy lifestyle as early as possible. Regular check-ups with your doctor should start in young adulthood to monitor risk factors like blood pressure and cholesterol.
Q: Is all chest pain related to the heart?
A: No, not at all. The chest contains many organs and tissues, including the lungs, esophagus, muscles, ribs, and nerves. Chest pain can be caused by acid reflux (heartburn), muscle strain from coughing or exercise, inflammation of the rib cartilage (costochondritis), lung issues like pneumonia, or shingles. However, because heart-related chest pain can be life-threatening, it’s the most serious potential cause and should always be ruled out by a medical professional.
Q: Can a healthy lifestyle completely prevent heart disease?
A: A healthy lifestyle—including a balanced diet, regular exercise, not smoking, and managing stress—is the single most effective way to reduce your risk of heart disease. It can prevent or delay the onset of cardiovascular problems for the vast majority of people. However, it cannot completely eliminate the risk, especially for those with strong genetic predispositions or other uncontrollable risk factors. The goal is to control what you can to give yourself the best possible odds for a long and healthy life.
Conclusion
Your heart is a remarkably resilient organ, but it is not invincible. The journey to a major cardiac event is often paved with small, subtle warnings that are all too easy to ignore. Moving beyond the stereotype of sudden, crushing chest pain and learning to recognize the quieter signs—like profound fatigue, shortness of breath with mild activity, referred pain in the jaw or back, dizziness, and swelling in the legs—is one of the most important things you can do for your long-term health. These are not just vague complaints; they are specific physiological signals that your cardiovascular system is under duress.
Listening to your body is not a sign of weakness or hypochondria; it is a profound act of self-care. Understand your personal risk factors, focus on managing the ones you can control, and build a partnership with your doctor. Do not dismiss what your body is trying to tell you. By being vigilant and proactive, you can intervene early, get the treatment you need, and protect the steady, life-giving beat of your heart for years to come.
***
Summary
This article, “Early Signs of Heart Disease: Go Beyond Chest Pain,” provides a comprehensive guide to understanding the subtle and often-overlooked symptoms of cardiovascular issues. It emphasizes that while classic chest discomfort (angina) is a critical sign, many early warnings are less dramatic and can be easily dismissed.
The main focus is on “atypical” signs, including unexplained, profound fatigue that isn’t relieved by rest and shortness of breath during minor daily activities. It details how pain from a struggling heart can be “referred” to other areas, such as the jaw, neck, back, or arms. Other key early indicators discussed are dizziness, lightheadedness, and swelling in the legs, ankles, and feet (edema), which signal problems with blood flow and fluid retention.
The article highlights that symptoms can present differently in women, who are more likely to experience nausea, indigestion, and extreme fatigue as primary signs. It provides a table of controllable versus uncontrollable risk factors (like high blood pressure vs. family history) to help readers assess their personal risk. Finally, it outlines common diagnostic tests and includes an FAQ section to address common concerns, urging readers to consult a doctor for any new or persistent symptoms rather than self-diagnosing. The core message is that early, proactive recognition of these subtle signs is crucial for preventing a major cardiac event.