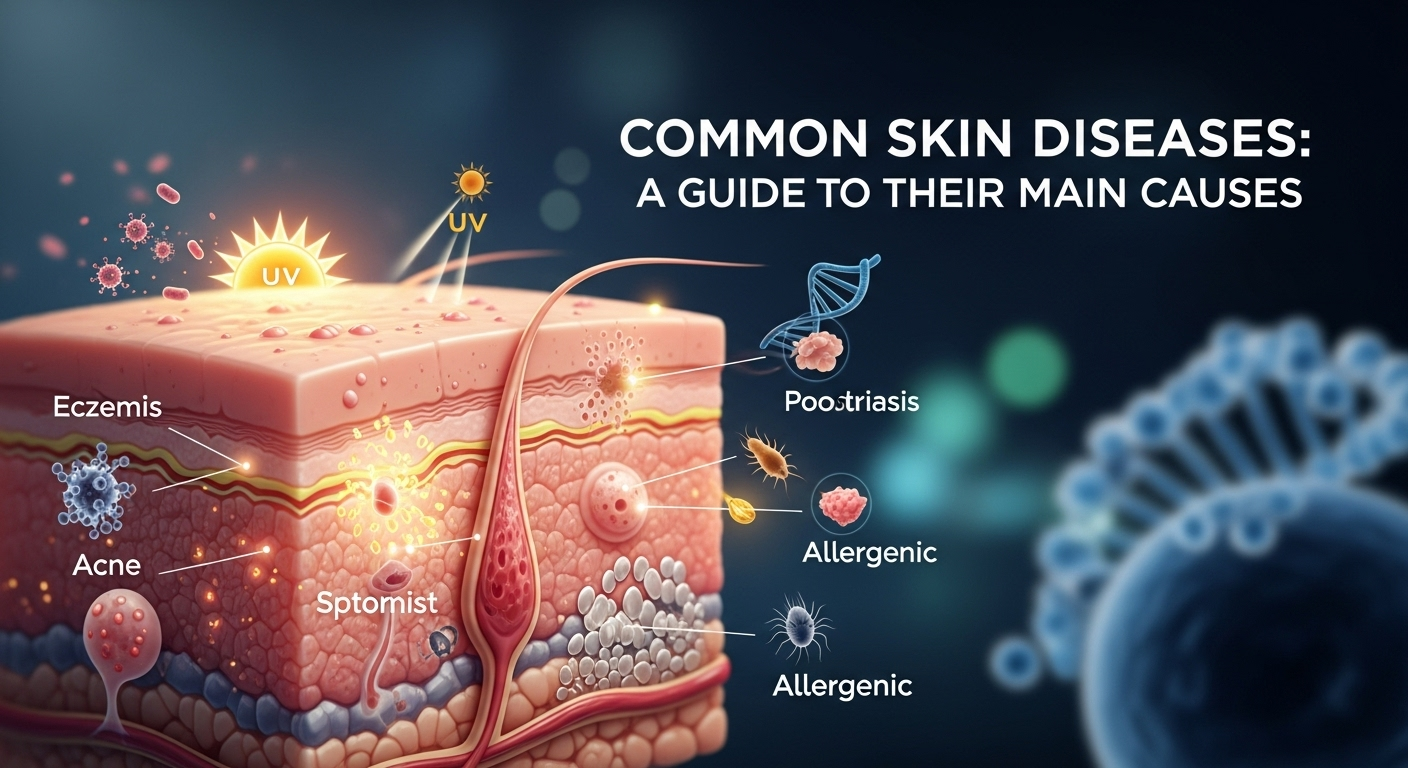
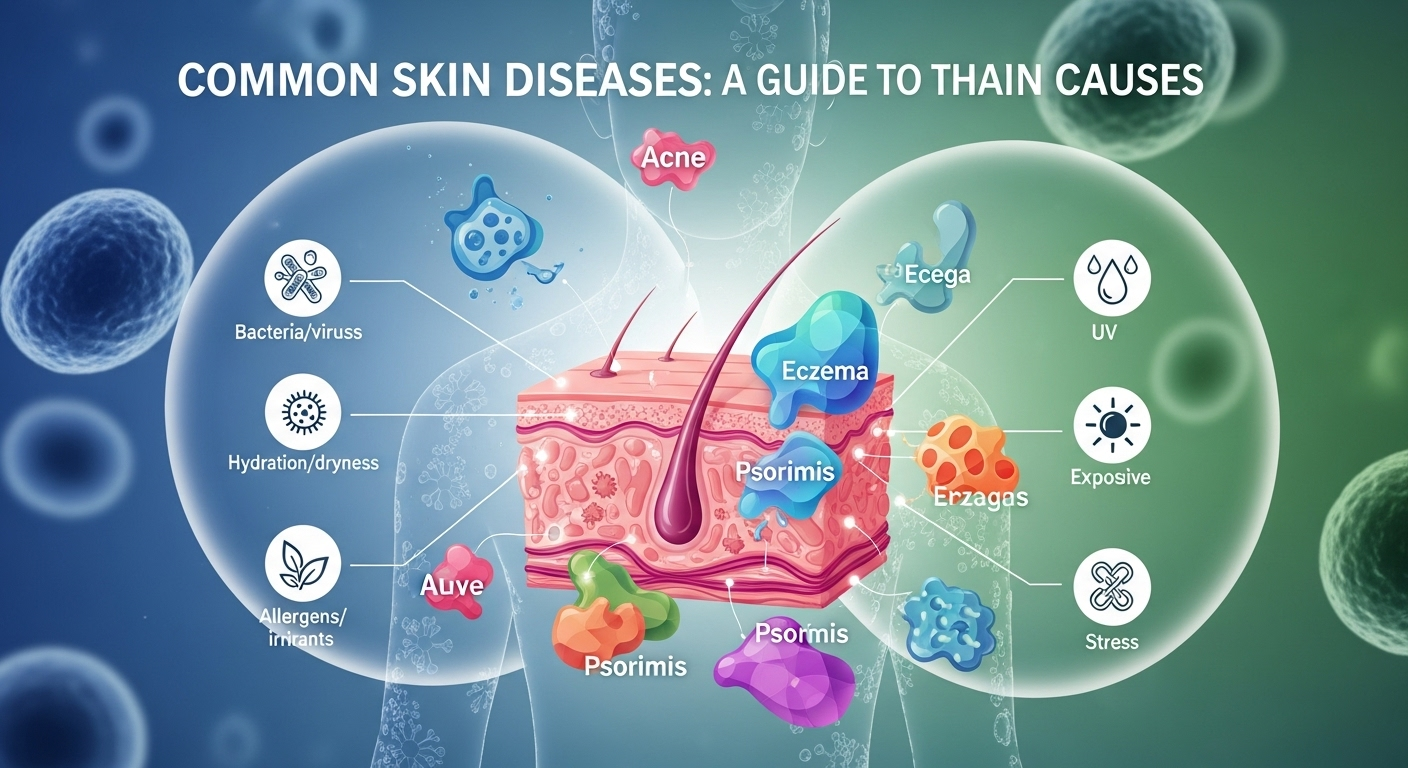
Our skin is more than just a protective outer layer; it's our body's largest organ and a visible indicator of our overall health. When it's healthy, it's a source of confidence. But when problems arise, they can be worrying, uncomfortable, and sometimes even debilitating. Understanding the vast world of common skin diseases and their causes is the first step toward effective management and peace of mind. This comprehensive guide will explore the primary factors behind prevalent skin conditions, from genetic predispositions and immune system malfunctions to environmental triggers and infectious agents, providing you with a clearer picture of what might be happening beneath the surface.
Table of Contents
ToggleUnderstanding the Basics of Skin Diseases
Before diving into specific conditions, it's essential to understand what constitutes a skin disease. Broadly, a skin disease, or dermatological condition, is any medical issue that affects the integumentary system—the system comprising the skin, hair, nails, and related glands. These conditions can cause a wide array of symptoms, including rashes, inflammation, itchiness, pain, changes in skin color, or abnormal growths. The impact of these diseases is often more than skin deep. They can significantly affect a person's self-esteem, mental health, and overall quality of life, making accurate information and proper care incredibly important.
The causes of skin diseases are incredibly diverse and often multifactorial, meaning several factors can contribute to a single condition. They can be broadly categorized into several groups. Genetic predispositions play a significant role in conditions like eczema and psoriasis, where a person inherits genes that make them more susceptible. The immune system is another major player; in autoimmune skin diseases, the body mistakenly attacks its own healthy skin cells. Furthermore, environmental factors such as allergens, irritants, sun exposure, and even stress can trigger or exacerbate many skin problems. Finally, infectious agents like bacteria, viruses, fungi, and parasites are responsible for a large number of contagious skin ailments.
It's also crucial to recognize the complexity and overlap between these causes. For instance, a person with a genetic predisposition to eczema might experience a flare-up only when exposed to a specific environmental irritant, such as a harsh soap or a change in weather. Similarly, a weakened immune system can make a person more vulnerable to bacterial or fungal infections. This intricate interplay is why diagnosing a skin condition is not always straightforward and why a "one-size-fits-all" approach to treatment is rarely effective. Understanding these underlying mechanisms is the cornerstone of dermatological science and the key to developing targeted, personalized treatment plans.
Inflammatory Skin Conditions: When the Body's Defenses Go Awry
Some of the most common and chronic skin disorders are inflammatory in nature. These conditions occur when the body's immune system becomes overactive or misdirected, leading to chronic inflammation, redness, swelling, and discomfort. While they are not contagious, they often have a genetic component and can be triggered by a variety of internal and external factors. Managing these conditions typically involves reducing inflammation and avoiding known triggers.
Eczema (Atopic Dermatitis)
Eczema, with atopic dermatitis being its most common form, is a condition characterized by dry, itchy, and inflamed skin. It often begins in childhood but can persist into or even start in adulthood. The hallmark symptom is an intense itch that, when scratched, leads to a red, weeping, or scaly rash—a cycle often referred to as the "itch-scratch cycle." This condition can appear anywhere on the body but is commonly found in the crooks of the elbows and knees, as well as on the hands, face, and neck.
The causes of eczema are a classic example of a complex interplay between genetics and environment. Many individuals with eczema have a genetic mutation in the gene responsible for creating filaggrin, a protein that helps maintain a healthy protective barrier on the skin. Without a sufficient amount of filaggrin, the skin loses moisture more easily and becomes more vulnerable to allergens and irritants. This compromised skin barrier, combined with an overreactive immune system that responds aggressively to these irritants, leads to the characteristic inflammation and itching of an eczema flare-up. Common triggers include dry air, harsh soaps, certain fabrics like wool, food allergies, and stress.
Psoriasis
Psoriasis is a chronic autoimmune disease that accelerates the life cycle of skin cells. Normally, skin cells grow and shed in about a month. In people with psoriasis, this process happens in just a few days. Because the body can't shed these excess cells quickly enough, they pile up on the surface of the skin, forming thick, red, inflamed patches covered with silvery scales. These patches, known as plaques, can be itchy and sometimes painful. The most common type is plaque psoriasis, but other forms can affect the scalp, nails, and even the joints (psoriatic arthritis).
The root cause of psoriasis lies within the immune system, specifically with T-cells, a type of white blood cell. In individuals with psoriasis, these T-cells are mistakenly triggered and become overactive. They begin to attack healthy skin cells as if they were fighting an infection or healing a wound. This autoimmune attack causes the rapid skin cell production and inflammation seen in psoriasis. Genetics play a strong role; if a close family member has psoriasis, your risk is higher. Triggers that can cause a flare-or even the initial onset—include stress, injury to the skin (known as the Koebner phenomenon), certain medications (like beta-blockers), and infections, particularly strep throat.
Rosacea
Rosacea is a common skin condition that causes persistent redness and visible blood vessels in the face. It may also produce small, red, pus-filled bumps. These signs and symptoms may flare up for weeks to months and then go away for a while. Rosacea is often mistaken for acne, an allergic reaction, or other skin problems. It is most common in middle-aged women with fair skin, but it can affect anyone. Over time, it can cause the skin, particularly on the nose, to thicken and enlarge, a condition known as rhinophyma.
The exact cause of rosacea remains a mystery, but researchers believe it's a combination of hereditary and environmental factors. A key theory involves neurovascular dysregulation, meaning there's an issue with how the nerves control the blood vessels in the face, causing them to dilate too easily and lead to flushing and redness. An overabundance of a microscopic mite called Demodex folliculorum, which normally lives on human skin, is also frequently observed in people with rosacea, though it's unclear if the mites are a cause or a result of the condition. Common triggers that can exacerbate rosacea are well-documented and include sun exposure, heat, stress, alcohol, spicy foods, and certain skincare products.
Gland-Related Disorders: Acne Vulgaris
Our skin is covered in tiny glands, primarily sebaceous (oil) glands and sweat glands. When these glands malfunction, it can lead to some of the most widespread skin issues. The most notorious of these is acne vulgaris, a condition that affects millions of people, not just teenagers, and is directly linked to the activity of the sebaceous glands.
The Complex Causes of Acne Vulgaris
Acne vulgaris is an inflammatory disorder of the pilosebaceous unit, which consists of a hair follicle and its associated sebaceous gland. It manifests as various lesions, including "blackheads" (open comedones), "whiteheads" (closed comedones), pimples (pustules), and deeper, painful cysts. While it's most prevalent during puberty due to hormonal surges, adult acne is increasingly common, particularly in women.
The development of acne is driven by four primary, interconnected factors. First is excess sebum (oil) production, which is largely influenced by hormones called androgens. Second is the abnormal shedding of skin cells (hyperkeratinization) inside the hair follicle, which causes the pore to become clogged. Third, this clogged, oily environment becomes a perfect breeding ground for a bacterium called Propionibacterium acnes (P. acnes), which proliferates. Finally, the body's inflammatory response to this bacterial overgrowth and the byproducts they produce causes the redness, swelling, and pain associated with a pimple. This entire cascade is why treatments often target multiple pathways, such as reducing oil, unclogging pores, and fighting bacteria and inflammation.
Infectious Skin Diseases: When Microbes Invade
A large category of skin diseases is caused directly by an invasion of microorganisms. These conditions are often contagious and are caused by fungi, bacteria, or viruses that breach the skin's protective barrier. Treatment typically involves antimicrobial, antiviral, or antifungal medications targeted at the specific invading organism.
Fungal Infections (Mycoses)
Fungal skin infections are caused by various types of fungi, with a group called dermatophytes being the most common culprit. These organisms thrive in warm, moist, and dark environments, which is why infections are common in areas like the feet, groin, and scalp. They feed on keratin, the protein found in skin, hair, and nails.
Common examples include Athlete's Foot (tinea pedis), characterized by scaling, itching, and cracking between the toes; Ringworm (tinea corporis), which despite its name is a fungus that creates a circular, ring-shaped rash on the body; and Jock Itch (tinea cruris), an itchy rash in the groin area. These infections are typically caused by direct contact with the fungus, either from an infected person, an animal, or a contaminated surface like a locker room floor or a shared towel. Good hygiene and keeping the skin dry are key preventative measures.
Bacterial Infections
Bacterial skin infections occur when bacteria, most commonly Staphylococcus aureus or Streptococcus pyogenes, enter the skin, usually through a cut, scrape, or insect bite. The severity can range from a minor issue to a life-threatening emergency, depending on the type of bacteria and the depth of the infection.
Two common bacterial infections are Impetigo and Cellulitis. Impetigo is a highly contagious infection, most common in young children, that causes red sores that can burst and develop honey-colored crusts. Cellulitis is a deeper infection of the skin and the underlying soft tissue. It appears as a red, swollen, warm, and tender area of skin that can spread rapidly. Cellulitis requires prompt medical attention, as the infection can spread to the bloodstream and become systemic. The main cause is always a break in the skin's barrier, allowing the bacteria that normally live harmlessly on the surface to invade deeper tissues.
| Feature | Eczema (Atopic Dermatitis) | Psoriasis | Rosacea |
|---|---|---|---|
| Primary Appearance | Dry, red, intensely itchy patches; can be weepy. | Thick, red plaques with silvery scales. | Persistent facial redness, flushing, visible blood vessels, bumps. |
| Common Location | Elbow/knee creases, hands, face, neck. | Elbows, knees, scalp, lower back. | Central face (cheeks, nose, forehead). |
| Core Cause | Genetic (filaggrin defect) + Immune overreaction + Barrier dysfunction. | Autoimmune disease (T-cell attack on skin cells). | Unknown; likely genetic + neurovascular dysregulation. |
| Key Sensation | Severe Itchiness | Itchiness, sometimes pain or burning. | Burning or stinging sensation. |
| Common Triggers | Allergens, irritants (soaps), dry air, stress. | Stress, skin injury, infection (strep), some medications. | Sun, heat, alcohol, spicy foods, stress. |
When to Seek Professional Help
With the vast amount of information available online, it can be tempting to self-diagnose a skin condition. However, this can be risky. Many skin diseases look alike to the untrained eye, but their causes and treatments are vastly different. Using the wrong treatment on a misdiagnosed condition can, at best, be ineffective and, at worst, make the problem more severe. A board-certified dermatologist is a medical doctor who specializes in diagnosing and treating more than 3,000 different diseases of the skin, hair, and nails.
You should make an appointment with a dermatologist or your primary care physician if you experience any of the following. First, if a rash or skin lesion appears suddenly, is severe, or covers a large part of your body. Second, if you have signs of an infection, such as fever, increasing pain, swelling, warmth, or pus. Third, if a condition is not improving with over-the-counter treatments or is getting worse. Finally, any new or changing mole should be evaluated immediately to rule out skin cancer.
Ultimately, a proper diagnosis is the most critical step toward relief. A dermatologist can perform a physical examination, take a detailed history, and, if necessary, perform a skin biopsy (taking a small sample of skin for analysis) to determine the exact cause of your problem. This ensures you receive the safest and most effective treatment plan tailored to your specific condition, leading to better outcomes and improved skin health in the long run.
Conclusion
The world of skin diseases is vast and complex, with causes ranging from our own genetic makeup and immune responses to the microscopic organisms and environmental factors that surround us every day. Conditions like eczema, psoriasis, and rosacea stem from internal inflammatory processes, while acne is a multifaceted issue of glands and blockages. Meanwhile, infectious diseases are a direct result of invasions by fungi, bacteria, and viruses.
While this guide provides a foundational understanding of these common issues, it is not a substitute for professional medical advice. The key takeaway is that your skin is a window into your overall health, and any persistent or worrying changes warrant a consultation with a healthcare professional. By seeking an accurate diagnosis from a dermatologist, you empower yourself to manage your condition effectively, alleviate discomfort, and take proactive steps toward achieving healthier, more resilient skin for years to come.
—
Frequently Asked Questions (FAQ)
Q: Can stress cause or worsen skin diseases?
A: Absolutely. Stress is a well-documented trigger and exacerbating factor for a wide range of skin conditions, including eczema, psoriasis, acne, and rosacea. When you are stressed, your body releases hormones like cortisol, which can increase inflammation and oil production, disrupt the skin's barrier function, and suppress the immune system, making you more susceptible to flare-ups and infections.
Q: Are all skin diseases contagious?
A: No, most of the common chronic skin diseases are not contagious. Inflammatory and autoimmune conditions like eczema, psoriasis, rosacea, and acne cannot be passed from person to person. However, skin diseases caused by infectious agents—such as ringworm (fungal), impetigo (bacterial), and warts (viral)—are contagious through direct contact or sharing contaminated items.
Q: How much does diet really affect my skin?
A: The link between diet and skin health is a growing area of research. For some conditions, the connection is clearer. For example, high-glycemic-index foods (like sugar and refined carbohydrates) have been shown to worsen acne in some individuals by spiking insulin and stimulating oil production. For inflammatory conditions like eczema or rosacea, certain foods can act as triggers for some people. Keeping a food diary can help you identify potential dietary triggers for your specific condition.
Q: What is the difference between a simple rash and a skin disease?
A: A "rash" is a general, descriptive term for a noticeable change in the texture or color of your skin. A simple rash might be a temporary reaction to an irritant, like contact dermatitis from a new lotion, and may resolve on its own. A "skin disease," on the other hand, is a diagnosed medical condition that is often chronic or recurring, such as psoriasis or eczema. Essentially, a rash is often a symptom of an underlying skin disease.
Q: What are the best general practices to protect my skin and prevent these conditions?
A: While you can't change your genetics, you can adopt habits to support overall skin health. These include: using a gentle, non-irritating cleanser; moisturizing daily to support the skin barrier; consistently wearing broad-spectrum sunscreen with an SPF of 30 or higher; managing stress through techniques like meditation or exercise; and avoiding known personal triggers, whether they are specific foods, allergens, or harsh products.
***
Article Summary
This comprehensive guide, "Common Skin Diseases: A Guide to Their Main Causes," provides an in-depth look at prevalent dermatological conditions. The article establishes that skin diseases are complex, often resulting from a mix of genetic, immune, environmental, and infectious factors. It categorizes and explains major skin problems, including inflammatory conditions like Eczema, an issue of barrier dysfunction and immune overreaction; Psoriasis, an autoimmune disease causing rapid cell turnover; and Rosacea, characterized by facial redness and flushing. The piece also details gland-related disorders, focusing on the four main causes of Acne Vulgaris. Furthermore, it covers infectious diseases caused by fungi (Ringworm), bacteria (Impetigo, Cellulitis), and viruses. A comparative table, an FAQ section, and a strong emphasis on seeking professional diagnosis from a dermatologist for any persistent or severe skin issue are included to provide actionable, trustworthy information for the reader.