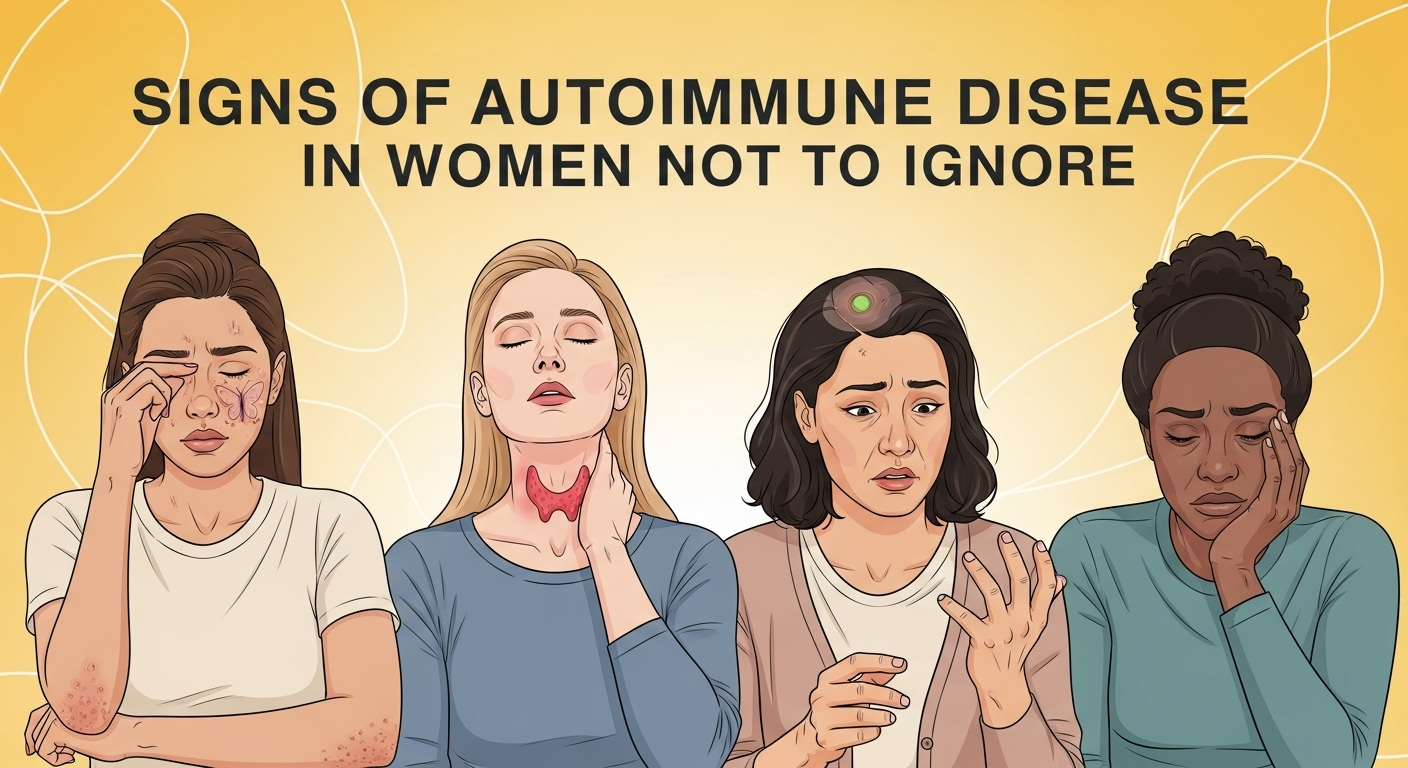
Your body sends you signals every day, but some are easier to ignore than others. A passing headache, a day of feeling tired, or a bit of bloating can all be dismissed as part of a busy life. However, when these seemingly minor issues become persistent, cluster together, or grow in intensity, they could be your body’s way of sounding an alarm. For women, these alarms can often point toward a complex and frequently misunderstood category of conditions. The symptoms of autoimmune disease in women are notoriously varied and often mimic other, less serious ailments, leading to long and frustrating diagnostic journeys. Understanding these signs is the first crucial step toward taking control of your health.
Table of Contents
ToggleUnderstanding Autoimmune Disease: When Your Body Becomes the Enemy
At its core, an autoimmune disease is a condition where your body's immune system, designed to protect you from foreign invaders like bacteria and viruses, mistakenly attacks its own healthy cells, tissues, and organs. Think of it as a case of friendly fire on a cellular level. Instead of targeting pathogens, the immune system creates autoantibodies that identify parts of your own body—like your joints, skin, or thyroid gland—as threats. This misguided assault leads to inflammation, damage, and a wide array of symptoms that can affect nearly every part of the body. There are over 80 different types of autoimmune diseases, including well-known conditions like rheumatoid arthritis, lupus, and multiple sclerosis.
The staggering reality is that autoimmune diseases disproportionately affect women. According to the National Institutes of Health (NIH), a staggering 75% of Americans with autoimmune diseases are women. Scientists are still working to understand the exact reasons for this significant gender disparity, but leading theories point to a combination of factors. Hormones, particularly estrogen, are believed to play a role in modulating the immune response. The genetic difference of having two X chromosomes, which carry a large number of immune-related genes, may also contribute to a more robust—and sometimes overactive—immune response in women compared to men.
This biological predisposition, combined with the fact that autoimmune symptoms are often vague and can overlap with numerous other conditions, makes the path to diagnosis exceptionally challenging. Many women report being told their symptoms are "all in their head," a result of stress, or simply a normal part of aging. This dismissal can lead to years of suffering without answers, allowing the underlying disease to progress. Therefore, recognizing the pattern of these symptoms and advocating for proper medical investigation is not just important; it's a critical act of self-care.
The Systemic Signs: Widespread Symptoms You Can't Pinpoint
Some of the most common and earliest signs of an autoimmune condition are not localized to one specific area. Instead, they are systemic, meaning they affect your entire body. These symptoms are often the most frustrating because they are non-specific and can be easily attributed to lifestyle factors like a demanding job, lack of sleep, or stress. However, their persistence and impact on your quality of life are key indicators that something more is at play.
- Persistent and Profound Fatigue
This isn’t the kind of tiredness that a good night’s sleep or a cup of coffee can fix. Autoimmune fatigue is a debilitating, whole-body exhaustion that can interfere with your daily activities, work, and social life. It can feel like you’ve run a marathon even when you’ve just woken up, or like you’re constantly wading through mud. The energy simply isn’t there, no matter how much you rest.
This profound fatigue is a direct result of the chronic inflammation coursing through your body. Your immune system is in a constant state of high alert, expending enormous amounts of energy to fight a perceived threat that is, in reality, your own tissue. This biological "war" drains your resources, leaving you feeling perpetually exhausted. If you find that rest does little to restore your energy levels and that fatigue is significantly impacting your ability to function, it's a major red flag that should not be ignored.
- Chronic Low-Grade Fever
A fever is a classic sign that your body is fighting something off. When you have a cold or the flu, a temporary high fever is expected. However, a persistent, low-grade fever—often hovering around 99°F to 101°F (37.2°C to 38.3°C)—that lasts for weeks or months without an obvious infection is a different matter. This is a hallmark of systemic inflammation.
This type of recurrent, low-grade fever indicates that your immune system is continuously activated. It's a sign that the body's inflammatory processes are humming in the background, a common feature of many autoimmune diseases, particularly during a "flare-up" when the disease becomes more active. Instead of dismissing it as "just feeling a bit warm," tracking your temperature and noting its persistence can provide a crucial piece of evidence for your doctor.
- Unexplained Weight Changes
Your weight can fluctuate for many reasons, but sudden or unexplained weight loss or gain without changes in your diet or exercise routine can signal an underlying autoimmune issue. The direction of the change often depends on the specific disease and the organ system it is affecting.
For example, conditions like celiac disease or inflammatory bowel disease (IBD) can damage the digestive tract, leading to malabsorption of nutrients and subsequent weight loss. Conversely, an autoimmune condition affecting the thyroid, such as Hashimoto's thyroiditis, can slow down your metabolism, leading to unexplained weight gain, puffiness, and difficulty losing weight. These changes are not about aesthetics; they are physiological signs that a core bodily system is not functioning correctly due to an immune attack.
Visible and Physical Manifestations: What You Can See and Feel
While systemic symptoms are felt throughout the body, many autoimmune diseases also present with physical signs that you can see on your skin or feel in your joints and muscles. These visible manifestations are often what finally prompt individuals to seek medical help, as they provide tangible proof that something is wrong.
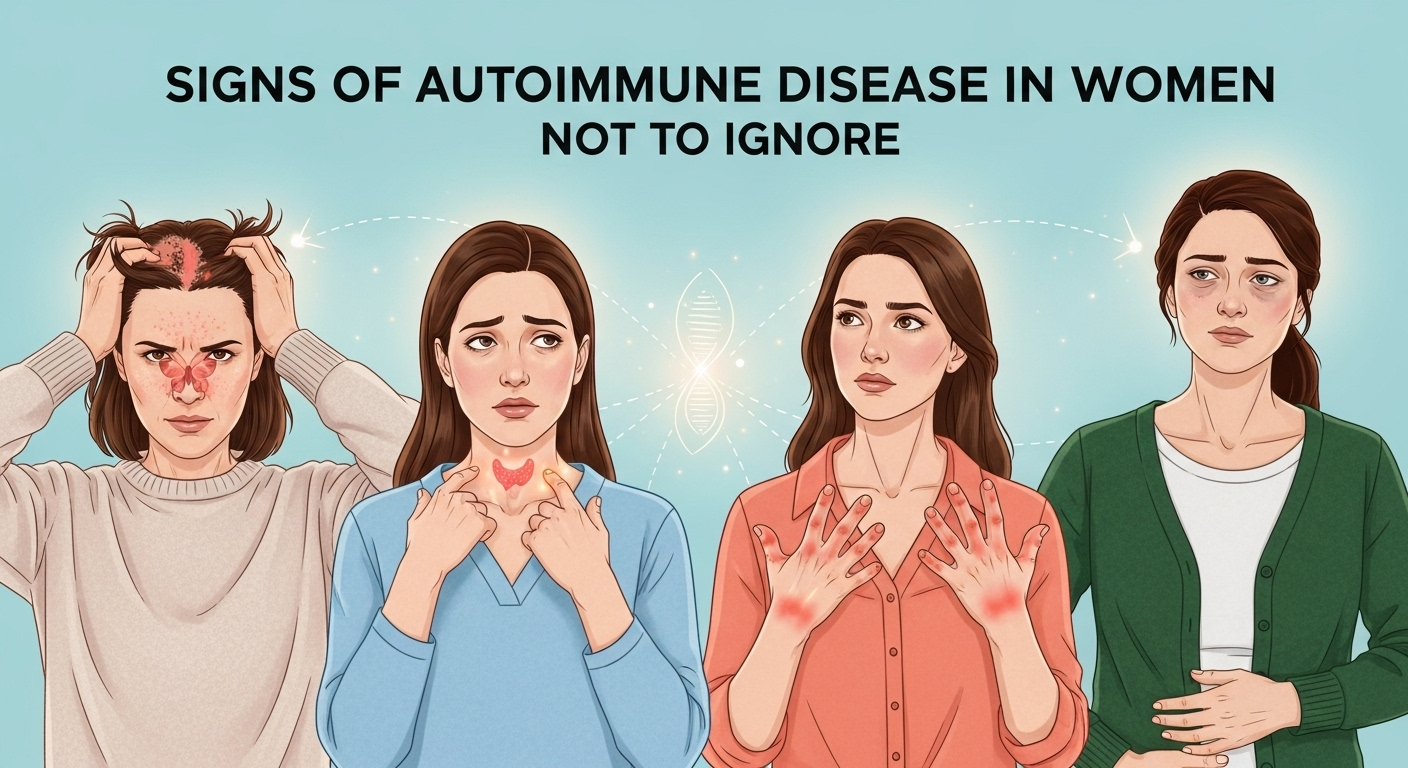
- Skin Issues: Rashes, Sores, and Sensitivity
The skin is often a window to the health of the immune system. Many autoimmune conditions are characterized by distinct skin manifestations because immune cells can mistakenly target skin cells. One of the most classic examples is the malar rash, or "butterfly rash," a reddish rash that spreads across the cheeks and bridge of the nose, commonly associated with lupus.
Other skin-related symptoms include scaly patches (psoriasis), hardened, tight patches of skin (scleroderma), sores in the mouth or nose, and photosensitivity, where sun exposure triggers or worsens rashes and other symptoms. If you develop a persistent rash that doesn't respond to typical over-the-counter treatments, or if your skin has become unusually sensitive to sunlight, it's a strong indicator that an internal inflammatory process is at play.
- Joint and Muscle Aches
Pain, stiffness, and swelling in the joints and muscles are cornerstone symptoms of many autoimmune diseases, most notably rheumatoid arthritis (RA). Unlike the mechanical pain from an injury, autoimmune joint pain is inflammatory. It is often symmetrical (affecting the same joints on both sides of the body), is typically worse in the morning, and can be accompanied by significant stiffness that lasts for more than 30 minutes upon waking.
This inflammation is caused by autoantibodies attacking the synovium, the lining of the joints, leading to swelling, pain, and eventually, erosion of the cartilage and bone. Similarly, generalized muscle pain and weakness, known as myalgia, can be a prominent feature in conditions like lupus and polymyositis. This isn't the normal soreness after a workout; it's a persistent ache that can make simple movements difficult.
- Hair Loss and Dryness
Your hair and moisture-producing glands can also become targets of an autoimmune attack. Patchy hair loss, known as alopecia areata, occurs when the immune system attacks the hair follicles, causing hair to fall out in small, round patches. Diffuse hair thinning is also common in lupus and thyroid-related autoimmune conditions.
Beyond hair, a condition called Sjögren's syndrome specifically targets the glands that produce saliva and tears. This leads to intensely dry eyes that may feel gritty or sandy, and a dry mouth that can make it difficult to swallow or speak and may increase the risk of dental cavities. This pervasive dryness is not simply a nuisance but a clear sign of a targeted autoimmune response.
The Neurological and Digestive Connection
The immune system's reach extends deep into the body's control centers: the nervous system and the digestive tract. The gut-brain-immune axis is a complex communication network, and when the immune system goes awry, it can disrupt both neurological function and digestive health, leading to a host of confusing and debilitating symptoms.
- Digestive Distress: Beyond a Simple Stomach Ache
The gastrointestinal (GI) tract is a major hub for immune activity. It’s no surprise, then, that it is a common site for autoimmune attacks. Symptoms can range from abdominal pain and cramping to chronic diarrhea, constipation, bloating, and blood in the stool. These are hallmark signs of inflammatory bowel disease (IBD), which includes Crohn’s disease and ulcerative colitis.
In celiac disease, the immune system reacts to gluten (a protein found in wheat, barley, and rye) by attacking the lining of the small intestine. This not only causes digestive upset but also impairs the body's ability to absorb vital nutrients, leading to a cascade of other health problems. If you experience persistent digestive issues that don't resolve with simple dietary changes, it's essential to consider an underlying autoimmune cause.
- Neurological Symptoms: Brain Fog, Numbness, and Tingling
One of the most disorienting symptoms of autoimmune disease is “brain fog.” This isn’t simple forgetfulness; it’s a frustrating cognitive impairment that can manifest as difficulty concentrating, poor memory, confusion, and a feeling of being mentally slow. This occurs when systemic inflammation affects the brain, disrupting neurotransmitter function.
More specific neurological symptoms can point toward diseases like Multiple Sclerosis (MS), where the immune system attacks the myelin sheath that protects nerve fibers. This can cause a range of symptoms, including numbness or tingling in the limbs (paresthesia), muscle weakness, vision problems, and issues with balance and coordination. Any new, unexplained neurological symptom, from brain fog to tingling fingers, warrants immediate medical attention.
Seeking a Diagnosis: Navigating the Medical System
Receiving an autoimmune diagnosis is often a marathon, not a sprint. Because the symptoms are so diverse and can evolve over time, it requires patience, persistence, and proactive participation from you, the patient. Being prepared can make the process smoother and lead to a faster, more accurate diagnosis.
- The Importance of Symptom Tracking
Your personal account is the most powerful tool in the diagnostic process. Before you even see a doctor, start keeping a detailed symptom journal. Do not underestimate the power of this data. Note what symptom you’re experiencing, when it started, how severe it is (on a scale of 1-10), how long it lasts, and what, if anything, seems to make it better or worse (e.g., stress, certain foods, lack of sleep, sun exposure).
This log transforms vague complaints like "I'm tired" into concrete data like "For the past three weeks, I've experienced 8/10 fatigue that is worst in the morning and not improved by 8 hours of sleep." This level of detail helps your doctor see patterns they might otherwise miss and provides a compelling case for further testing. Bring this journal to every appointment.
- Key Diagnostic Tests
While there is no single test for most autoimmune diseases, a combination of blood tests can provide important clues. Your doctor will likely start with tests that look for general markers of inflammation, such as C-Reactive Protein (CRP) and Erythrocyte Sedimentation Rate (ESR).
A crucial next step is often the Antinuclear Antibody (ANA) test. A positive ANA test indicates the presence of autoantibodies, which are a hallmark of autoimmunity, particularly in conditions like lupus. While a positive ANA doesn't confirm a specific disease (some healthy people can have a positive ANA), it strongly suggests that an autoimmune process is at play and warrants investigation by a specialist. Depending on your specific symptoms, your doctor may order more specific antibody tests to look for rheumatoid factor (for RA), anti-TPO antibodies (for Hashimoto's), or others.
| Common Autoimmune Disease in Women | Primary Target | Key Distinguishing Symptoms |
|---|---|---|
| Lupus (SLE) | Multiple organs (skin, joints, kidneys, brain) | Butterfly-shaped facial rash, photosensitivity, fatigue, joint pain |
| Rheumatoid Arthritis (RA) | Lining of joints (synovium) | Symmetrical joint swelling and pain, prolonged morning stiffness |
| Hashimoto's Thyroiditis | Thyroid gland | Fatigue, weight gain, cold intolerance, hair loss, depression |
| Multiple Sclerosis (MS) | Myelin sheath of nerves (brain and spinal cord) | Numbness/tingling, muscle weakness, vision problems, balance issues |
Frequently Asked Questions (FAQ)
Q: Why are autoimmune diseases so much more common in women?
A: The exact reason is still being researched, but it's believed to be a combination of hormonal, genetic, and environmental factors. Women's hormones, particularly estrogen, can influence the immune response. Additionally, women have two X chromosomes, which contain a high number of immune-regulating genes, potentially leading to a stronger and sometimes overzealous immune system.
Q: Can stress cause or trigger an autoimmune disease?
A: While stress doesn't directly cause an autoimmune disease, it is a well-known and powerful trigger for flare-ups. For individuals with a genetic predisposition, a period of intense physical or emotional stress can sometimes precede the initial onset of symptoms. Managing stress through techniques like mindfulness, meditation, and gentle exercise is a critical part of managing any autoimmune condition.
Q: Is there a cure for autoimmune diseases?
A: Currently, there is no cure for most autoimmune diseases. However, there are many highly effective treatments available that can manage symptoms, reduce inflammation, and prevent long-term damage. The goal of treatment is to achieve remission, a state where the disease is inactive and symptoms are minimal or absent. Treatment plans are highly individualized and may include medication, lifestyle changes, and dietary adjustments.
Q: What is the first step I should take if I suspect I have an autoimmune disease?
A: The first and most important step is to schedule an appointment with your primary care physician. Before you go, start a detailed symptom journal as described above. Be prepared to clearly and calmly advocate for yourself. Present your documented symptoms and specifically ask if an autoimmune condition could be a possibility. A good doctor will take your concerns seriously and begin the appropriate blood work or refer you to a specialist, such as a rheumatologist.
Conclusion
The signs of autoimmune disease in women are complex, often subtle, and easy to dismiss. From the profound fatigue that seeps into every corner of your life to the mysterious rash that appears after a day in the sun, these symptoms are your body's attempt to communicate a deep-seated imbalance. Ignoring them, or allowing them to be dismissed by others, can delay diagnosis and lead to progressive damage.
Listening to your body is an act of empowerment. By recognizing these signs, tracking your symptoms diligently, and advocating for yourself within the medical system, you can take the first and most critical step on the path to getting answers. A diagnosis, while potentially intimidating, is not an end point; it is the beginning of understanding, management, and reclaiming your quality of life. Your symptoms are real, they are valid, and they deserve to be investigated.
***
Article Summary
"Signs of Autoimmune Disease in Women Not to Ignore" is a comprehensive guide detailing the varied and often overlooked symptoms of autoimmune conditions, which disproportionately affect women. The article explores a wide range of signs, from systemic issues like profound fatigue and low-grade fevers, to visible manifestations such as skin rashes and joint pain, and even neurological and digestive problems. It emphasizes the importance of symptom tracking and self-advocacy in navigating the often-difficult diagnostic process. By providing actionable advice, a comparative table of common diseases, and an FAQ section, the article aims to empower women to recognize these crucial signals, seek timely medical help, and begin the journey toward diagnosis and effective management.