A Guide to Understanding the Stages of Kidney Disease
Your kidneys are among the body's most vital and hardworking organs. Functioning as sophisticated filtration systems, they tirelessly cleanse your blood, manage fluid balance, regulate blood pressure, and support bone health, all while operating silently in the background. However, when their function begins to decline gradually over time, a condition known as Chronic Kidney Disease (CKD) can develop. This condition is often progressive, moving through distinct phases that can be confusing and alarming. Gaining a clear and comprehensive perspective is the first and most crucial step toward managing the condition effectively. This comprehensive guide is designed to demystify the process, providing a clear path to understanding the stages of kidney disease and empowering you with the knowledge to navigate your health journey.
What is Chronic Kidney Disease (CKD)?
Chronic Kidney Disease, often abbreviated as CKD, is a long-term condition characterized by the gradual loss of kidney function over months or years. Unlike Acute Kidney Injury (AKI), which involves a sudden loss of kidney function, CKD is a slow and often silent decline. The primary role of the kidneys is to filter waste products and excess fluid from the blood, which are then excreted in the urine. When the kidneys are damaged, they become less efficient at this filtration process, leading to a build-up of waste and fluid in the body that can cause a cascade of health problems.
The importance of the kidneys cannot be overstated. Beyond filtration, they perform several critical functions:
- Regulating blood pressure by managing fluid levels and releasing hormones.
- Producing an active form of Vitamin D, which is essential for bone health and calcium absorption.
<strong>Controlling the production of red blood cells</strong> through the hormoneerythropoietin*.
- Balancing the body&#x27;s electrolytes, such as sodium, potassium, and phosphate.
When CKD develops, all of these functions can become impaired. The disease is "staged" based on the level of kidney function remaining. This staging system helps doctors determine the severity of the disease, predict its rate of progression, and develop an appropriate management plan. By understanding which stage you or a loved one is in, you can better grasp the immediate health priorities and the long-term outlook, making you an active participant in your own care.
The Key Metric: Understanding Glomerular Filtration Rate (eGFR)
The cornerstone for staging kidney disease is a measurement called the Glomerular Filtration Rate, or GFR. The glomeruli are tiny filters within your kidneys—millions of them—that perform the initial step of cleaning your blood. The GFR is a measure of how much blood these filters clean each minute. A healthy pair of kidneys can filter approximately 120 milliliters (mL) of blood per minute. A direct GFR measurement is complex, so doctors typically use a formula to calculate an estimated Glomerular Filtration Rate (eGFR).
To calculate your eGFR, your doctor will order a simple blood test that measures the level of creatinine, a waste product generated from muscle metabolism. This creatinine level is then plugged into a mathematical formula along with other variables like your age, sex, and body size. Historically, race was also a factor in the calculation, but modern guidelines are moving away from this practice to promote health equity and improve accuracy. The resulting eGFR number gives your healthcare provider a clear and reliable estimate of your kidney function percentage.
The eGFR is the single most important number for staging CKD. Think of it as a percentage score for your kidneys. An eGFR of 75 means you have approximately 75% of your kidney function. As the eGFR number decreases, it signifies that the kidneys are becoming less effective at their job. This number allows doctors to classify the disease into one of five stages, track its progression over time, and make critical decisions about treatment, diet, and when to prepare for advanced therapies like dialysis or transplantation.
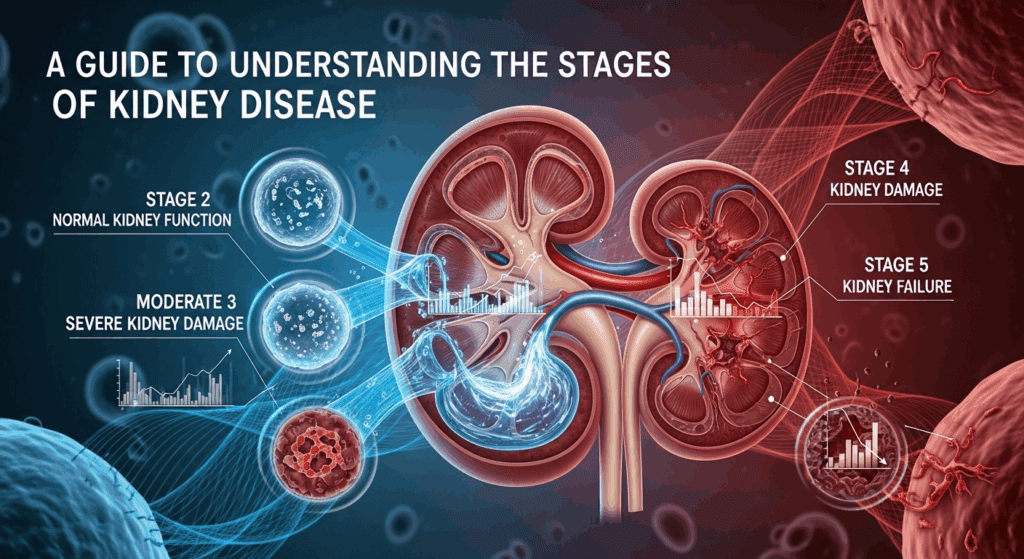
A Detailed Breakdown of the 5 Stages of Kidney Disease
Understanding what each stage means is vital for managing expectations and taking the right actions at the right time. The stages are primarily defined by the eGFR level, but the presence of kidney damage (such as protein in the urine, known as albuminuria) is also a critical factor, especially in the early stages.
Stage 1: Kidney Damage with Normal or High GFR
In Stage 1 CKD, the eGFR is 90 mL/min or higher, which is considered normal or even high kidney function. A person is only diagnosed with Stage 1 if they have other markers of kidney damage. This evidence could be the persistent presence of protein or blood in the urine, abnormalities detected on an ultrasound or CT scan (like polycystic kidney disease), or a family history of genetic kidney disease. Essentially, the kidneys are still working at or near full capacity, but there is underlying damage that signals a problem.
Because kidney function is still good, symptoms are almost always absent in Stage 1. Most people are completely unaware they have a problem unless it is discovered incidentally during routine urine or blood tests for another condition. The primary goal of management at this stage is not to treat kidney failure but to aggressively manage the underlying cause of the damage to slow or halt its progression. This often involves strict control of blood pressure, managing blood sugar levels in people with diabetes, adopting a healthy lifestyle, and avoiding medications that can harm the kidneys (nephrotoxic drugs).
Stage 2: Kidney Damage with Mildly Decreased GFR
Stage 2 CKD is defined by an eGFR between 60 and 89 mL/min, coupled with evidence of kidney damage. This represents a mild decline in kidney function. Just like in Stage 1, the kidneys are still performing their essential tasks relatively well, and the body can effectively compensate for the slight loss in filtration capacity. It is a critical juncture where proactive management can have a significant long-term impact on the health of your kidneys.
Symptoms remain rare in Stage 2, although some individuals might experience high blood pressure as one of the first signs of trouble. The focus of treatment remains centered on preservation. Your doctor will work with you to implement strategies to protect your remaining kidney function and slow the rate of decline. This includes the same foundational principles as Stage 1: controlling blood pressure and diabetes, eating a kidney-friendly diet (often low in sodium), quitting smoking, and maintaining a healthy weight. Regular monitoring of eGFR and urine protein levels becomes increasingly important to track the disease's trajectory.
Stage 3: Moderately Decreased GFR (Stage 3a and 3b)
Stage 3 is a significant turning point in Chronic Kidney Disease, as it is the point where symptoms and complications often begin to emerge. It is defined by an eGFR between 30 and 59 mL/min and is further divided into two sub-stages to provide more precise information about the level of function. Stage 3a corresponds to an eGFR of 45-59 mL/min, while Stage 3b indicates a more advanced, moderate loss of function with an eGFR of 30-44 mL/min.
As kidney function declines to this level, waste products start to build up more noticeably in the blood. This can lead to a variety of symptoms, including fatigue, fluid retention (edema) in the legs and feet, changes in urination (more or less frequent), and back pain. More importantly, this is the stage where common complications of CKD become prevalent. These include:
<strong>Anemia:</strong> The kidneys produce lesserythropoietin*, leading to a lower red blood cell count and causing weakness and fatigue.
- Bone Disease: Impaired activation of Vitamin D and poor phosphate filtering disrupt calcium balance, weakening bones.
- High Blood Pressure: Worsening blood pressure which, in turn, can further accelerate kidney damage.
- Your healthcare team will likely become more involved, potentially including a nephrologist (kidney specialist) and a renal dietitian to help manage these complications with medications and a more specific diet.
Stage 4: Severely Decreased GFR
Stage 4 CKD represents a severe loss of kidney function, with an eGFR between 15 and 29 mL/min. At this point, the kidneys have lost a significant amount of their ability to filter blood, and the build-up of waste products (uremia) becomes much more pronounced. It is highly likely that a person in Stage 4 will be experiencing noticeable symptoms and complications that impact their daily quality of life.
The symptoms seen in Stage 3 often become more severe and may be joined by others like nausea, loss of appetite, a metallic taste in the mouth, difficulty concentrating, and nerve problems. Management becomes highly intensive, focusing on treating these symptoms and complications aggressively. Stage 4 is also known as the "pre-dialysis" stage. It is a critical time for education and preparation for what is known as renal replacement therapy. Your medical team will begin extensive conversations with you about your options for when your kidneys fail, which include different types of dialysis (hemodialysis and peritoneal dialysis) and kidney transplantation.
Stage 5: Kidney Failure (End-Stage Renal Disease)
Stage 5 CKD is defined by an eGFR of less than 15 mL/min. This is also known as End-Stage Renal Disease (ESRD) or established kidney failure. At this point, the kidneys have either failed completely or are very close to failing. They can no longer remove waste and excess fluid from the body on their own to sustain life. Without treatment, toxins would build up to fatal levels. The symptoms are severe and can include intense itching, muscle cramps, severe nausea and vomiting, and significant swelling.
Once a person reaches Stage 5 CKD, life-sustaining treatment is required. There are two primary options for renal replacement therapy:
- Dialysis: A medical procedure that artificially filters the blood. Hemodialysis uses a machine to filter blood outside the body, typically at a clinic a few times a week. Peritoneal dialysis uses the lining of your own abdomen (peritoneum) to filter blood inside the body and can often be done at home.
- Kidney Transplant: A surgical procedure to place a healthy kidney from a living or deceased donor into your body. A successful transplant is the most effective treatment for kidney failure, offering the best quality of life, but it requires finding a suitable donor and taking lifelong anti-rejection medications.
—
<h3>Summary Table of CKD Stages</h3>

| Stage | eGFR (mL/min/1.73m²) | Kidney Function | Description & Management Focus |
|---|---|---|---|
| Stage 1 | ≥ 90 | Normal or High | Presence of kidney damage. Focus is on treating underlying conditions (e.g., diabetes, hypertension) to slow progression. |
| Stage 2 | 60–89 | Mildly Decreased | Mild loss of function with kidney damage. Focus on lifestyle changes and protecting remaining function. Monitor progression. |
| Stage 3a | 45–59 | Mild to Moderate | Moderate loss of function. Symptoms may begin. Complications like anemia and bone disease are monitored. Management becomes more active. |
| Stage 3b | 30–44 | Moderate to Severe | More significant loss. Complications are more likely. Consultation with a nephrologist and dietitian is often recommended. |
| Stage 4 | 15–29 | Severely Decreased | Severe loss of function. Symptoms are common. Intensive management of complications. Preparation for dialysis or transplant begins. |
| Stage 5 | < 15 | Kidney Failure | End-Stage Renal Disease (ESRD). Requires dialysis or a kidney transplant to sustain life. |
Symptoms and Complications Across the Stages
One of the most challenging aspects of Chronic Kidney Disease is its silent nature in the early stages. Many people with Stage 1, 2, or even early Stage 3 CKD have no idea there's an issue because their bodies are highly effective at compensating for the initial loss of function. This is why regular health screenings, especially for those with risk factors like diabetes, high blood pressure, or a family history of kidney disease, are so crucial for early detection.
As the disease progresses into the later stages (late Stage 3, Stage 4, and Stage 5), symptoms become more apparent and can significantly affect a person's well-being. These symptoms are primarily caused by the build-up of waste products and fluid in the body. Common signs to watch for include:
- Fatigue and weakness: Often linked to anemia.
<strong>Swelling (edema*) in the feet, ankles, hands, or face due to fluid retention.
- Changes in urination: Urinating more or less often, especially at night; foamy or bubbly urine (a sign of protein).
- Shortness of breath: Caused by fluid build-up in the lungs.
- Poor appetite, nausea, and vomiting.
- A metallic taste in the mouth or ammonia breath.
<strong>Persistent itching (pruritus*).
- Muscle cramps or twitching.
Beyond these direct symptoms, CKD gives rise to several serious systemic complications. The most common include anemia, where the body doesn't produce enough red blood cells; mineral and bone disorder, where bones become weak and brittle while calcium can deposit in blood vessels; and cardiovascular disease. In fact, people with CKD are far more likely to die from heart disease and stroke than from kidney failure itself, highlighting the critical importance of managing blood pressure and cholesterol.
Management and Treatment Strategies for CKD
While there is no cure for most forms of Chronic Kidney Disease, there is a great deal that can be done to manage the condition, slow its progression, and maintain a high quality of life. The treatment strategy is tailored to the specific stage of the disease and the individual's overall health.
Lifestyle and Dietary Changes
Lifestyle is the foundation of CKD management at every stage. For many, a diagnosis serves as a powerful motivator to adopt healthier habits. A renal dietitian is an invaluable resource who can help create a personalized eating plan. Key dietary adjustments often include:
- Reducing Sodium: To help control blood pressure and fluid retention.
- Managing Potassium and Phosphorus: These minerals can build up to dangerous levels in later-stage CKD.
- Monitoring Protein Intake: Too much protein can strain the kidneys, but too little can lead to malnutrition. The right amount depends on the stage of CKD and whether the person is on dialysis.
- Limiting Fluids: In later stages, fluid intake may need to be restricted to prevent swelling and heart strain.
- Other crucial lifestyle changes include quitting smoking, limiting alcohol, and engaging in regular physical activity as approved by your doctor.
Medical Treatments and Medications
Medication plays a pivotal role in slowing the progression of CKD and managing its complications. The primary goal is to control the underlying causes, most commonly diabetes and high blood pressure. Medications like ACE inhibitors (Angiotensin-Converting Enzyme inhibitors) and ARBs (Angiotensin II Receptor Blockers) are cornerstones of treatment as they both lower blood pressure and provide direct protection to the kidneys by reducing pressure inside the glomeruli.
More recently, a class of diabetes drugs known as SGLT2 inhibitors has revolutionized CKD care. They have been shown to significantly slow the progression of kidney disease in people both with and without diabetes. Other medications are used to manage complications:
- Iron supplements and erythropoiesis-stimulating agents (ESAs) to treat anemia.
- Phosphate binders to control phosphorus levels.
- Statins to manage high cholesterol and reduce cardiovascular risk.
- Active Vitamin D to support bone health.
Preparing for Kidney Failure
For individuals in Stage 4 and progressing toward Stage 5, the focus of medical care expands to include preparation for renal replacement therapy. This is a journey that requires time, education, and shared decision-making between the patient, their family, and the healthcare team. The goal is to make a smooth and planned transition to treatment, rather than an emergency start.
This process involves understanding the pros and cons of each modality. Hemodialysis offers a structured schedule but requires travel to a center and can be physically draining. Peritoneal dialysis provides more flexibility and can be done at home, but it requires a high level of self-care and carries a risk of infection. A kidney transplant offers the best chance at a near-normal life but involves major surgery and a potential waiting period for a suitable organ. For some, particularly the very elderly or those with other severe illnesses, a conservative, non-dialytic approach focusing on quality of life may also be an appropriate choice.
—
<h2>Frequently Asked Questions (FAQ)</h2>
Q: Can Chronic Kidney Disease be reversed?
A: In most cases, the damage that causes Chronic Kidney Disease is permanent and cannot be reversed. However, by managing the underlying causes (like blood pressure and diabetes) and adopting a kidney-friendly lifestyle, you can significantly slow down the progression of the disease and preserve your remaining kidney function for many years.
Q: What is the difference between Chronic Kidney Disease (CKD) and Acute Kidney Injury (AKI)?
A: The main difference is time. CKD is a long-term condition where kidney function is lost gradually over months or years. AKI is a sudden episode of kidney failure or damage that happens within a few hours or a few days. While AKI can sometimes be reversed if treated quickly, it can also lead to CKD.
Q: How often should I get my kidneys checked?
A: If you are at high risk for kidney disease—meaning you have diabetes, high blood pressure, heart disease, or a family history of kidney failure—you should have your eGFR and a urine test for protein checked at least once a year. If you have no risk factors, your doctor may check it as part of routine blood work.
Q: Does Stage 3 kidney disease always lead to kidney failure?
A: No, not at all. Many people with Stage 3 CKD are able to maintain that level of function for the rest of their lives with proper management. The goal of treatment at this stage is to stabilize kidney function and halt or dramatically slow any further decline, preventing the progression to Stages 4 and 5.
Q: What are the most important foods to avoid with kidney disease?
A: This depends heavily on your stage of disease and your specific lab results. Generally, a kidney-friendly diet involves limiting sodium (found in processed foods, canned soups, and fast food), potassium (found in bananas, oranges, potatoes), and phosphorus (found in dairy, dark colas, and processed meats). It is essential to work with a renal dietitian to create a safe and effective eating plan for you.
—
Conclusion
The journey through Chronic Kidney Disease can feel overwhelming, but knowledge is a powerful tool for transforming fear into action. Understanding the stages of kidney disease, from the silent beginnings of Stage 1 to the life-altering reality of Stage 5, provides a clear framework for you and your healthcare team to work together. Each stage presents a unique set of challenges and goals, but the overarching theme remains the same: proactive management is key. Early detection through regular screenings, diligent control of underlying conditions like diabetes and hypertension, and an unwavering commitment to a kidney-friendly lifestyle can profoundly alter the course of this disease. While a diagnosis of CKD is serious, it is not a final verdict. By taking control of your health, asking questions, and following your treatment plan, it is possible to slow progression, manage symptoms, and live a full and meaningful life at every stage.
***
Summary of the Article
This comprehensive guide explores the five stages of Chronic Kidney Disease (CKD), a condition defined by the gradual loss of kidney function over time. Staging is primarily based on the estimated Glomerular Filtration Rate (eGFR), a measure of how well the kidneys are filtering blood. The article provides a detailed breakdown of each stage: Stage 1 (normal eGFR with kidney damage), Stage 2 (mild loss), Stage 3 (moderate loss, where symptoms may start), Stage 4 (severe loss, requiring preparation for future treatment), and Stage 5 (kidney failure, requiring dialysis or transplant). It emphasizes that early stages are often asymptomatic, highlighting the importance of screening for at-risk individuals. The guide also covers common symptoms, complications like anemia and bone disease, and a three-pronged management approach involving lifestyle/dietary changes, medical treatments (such as ACE inhibitors and SGLT2 inhibitors), and preparation for renal replacement therapy. The ultimate goal of understanding and managing CKD is to slow its progression, treat complications, and empower patients to maintain the best possible quality of life.
